05 Jul The Clinic of the Future
This this post was originally posted here
The potential stalling of MDMA Assisted Therapy approval for many in the psychedelic space is a ‘come-to-Jesus’ moment.
“Wait, not everyone wants potent, innovative treatment options for debilitating mental health conditions?1”
Similarly, Spravato continues to have issues in the UK as the NICE folks at the NHS denied coverage for Spravato yet again2.
This uneasiness with new and stigmatized treatment methods is not limited to psychedelics.
Last week, a clinical study of ketogenic therapy—a promising treatment option for mental health and neuropsychiatric conditions—was shut down by the Maryland State Health Department, citing a new policy that will not allow any research other than federally funded research.
Despite these examples of our institutions’ deeply entrenched Status Quo Bias, the momentum of innovation and ‘new ways of seeing’ is unstoppable.
This has been the theme of our Emergent Paradigm series, in which we’ve touched on some of the concurrent innovations that are coming alongside psychedelics, including Metabolic Psychiatry, Neurostimulation, the Bayesian Brain, and the Predictive Mind Hypothesis, and the Contemplative Renaissance.3
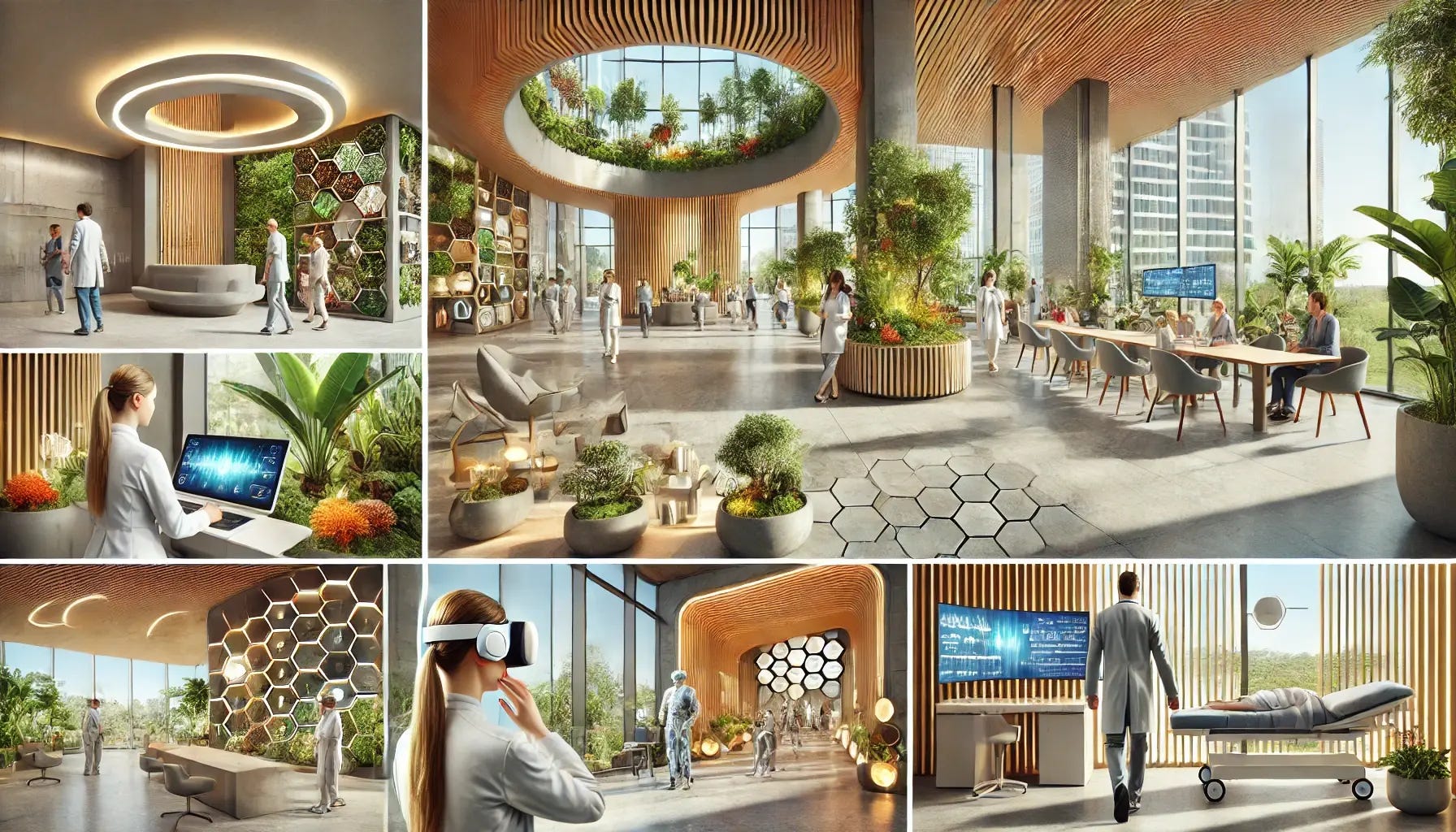
Today, I want to bring these things together to offer a view of the future that is waiting to be born—despite the inherent challenges—The Clinic of the Future.
The Clinic of the Future
Looking at the reserach, technologies, and treatment paradigms that are under development or in the early stages of distribution, we can see that future treatment approaches will fall into four categories:
- Relational
- Experiential
- Energetic
- Metabolic
The clinic of the future will operationalize treatments from each category to create robust and effective protocols.
Let’s take a look at each.
Relational
This is, in my estimation, the most critical category.
Despite exciting technologies, promising strategies, and new drugs, they will need to be deployed to foster connection with ourselves and others.
Of course, this category includes the doctor-patient relationship and the therapeutic alliance with a therapist or counselor. However, it also entails embedding within a group with a shared purpose or identity.
Throughout history, this has been the province of religion and other Third Spaces, but in our increasingly secular world, it has been replaced by politics and brand/celebrity affinity.
But there are bright spots in this domain—places where people convene to find meaning and connection and to lift each other up.
A few that come to mind are the 12 Step Programs, CrossFit, and Othership.
So, the clinic of the future will prioritize social connectedness with clinical and therapy staff, peer support, and partner with social programs beyond the clinic walls.
Experiential
Experiential therapies include psychedelics as well as multisensory immersive experiences like virtual reality, haptic stimuli, algorithmically programmed light and sound, and thermal conditioning—deliberate hyperthermia and cold water immersion.
The value of experiential therapies is their ability to recalibrate maladaptive patterns of perception that lead to unnecessary suffering.
The brain is the organ of prediction and protection. The chief aim is to ensure survival by predicting future states and scenarios and being prepared for them.
Nearly all of the difficult-to-treat mental health conditions are predicated on disruption or miscalibration of the nervous system’s ability to perceive and assign threat value to incoming sensory information.
Experiential therapies that support a recalibration of this process will be an invaluable toolset in holistic, patient-centered care.
Energetic
This is the category of brain stimulation by various means.
It includes currently available treatments like Transcranial Magnetic Stimulation and Vagus Nerve Stimulation but will soon include many more approaches.
Chief among them coming down the pike is a promising approach called Transcranial Focused Ultrasound (FUS).
tFUS is a non-invasive form of neurostimulation that uses ultrasound waves to target tissue deep within the brain. Unlike traditional ultrasound, tFUS focuses these waves to a precise point, allowing for targeted treatment without surgical intervention. This technology has potential applications in treating various neurological and psychiatric conditions.
The procedure involves passing ultrasound waves through the skull to reach specific brain regions to modulate neural activity.
Other categories include neuromodulation through non-invasive and minimally invasive bioelectronics, photobiomodulation (PBM), and transcranial direct current stimulation.
Not all of these treatment categories may become clinically viable, but many more will continue to emerge and prove useful.
Metabolic
The theory that many mental illnesses are downstream of metabolic dysfunction suggests that altered metabolism in the brain can explain the symptoms of mental disorders.
Christopher Palmer, the Harvard psychiatrist and founder of the Metabolic and Mental Health Program at Mass General, writes:
“…we have arrived at our common thread, the underpinning factor that lets us answer our tangled questions about causes and treatments, symptoms and overlaps. Mental disorders—all of them—are metabolic disorders of the brain.”
Metabolic therapies, specifically the ketogenic diet, have been found to improve brain health through improved mitochondria function, oxidative stress, and inflammation pathways and support neural network stability—all of which have the effect of reducing symptoms associated with a number of conditions, including depression, anxiety, and schizophrenia.
In May, researchers published a case series titled Complete remission of depression and anxiety using a ketogenic diet: case series.
The authors note:
“Complete remission of major depression and generalized anxiety disorder occurred within 7–12 weeks of therapeutic nutritional ketosis during treatment with a personalized animal-based ketogenic diet in adults with complex comorbid depression and anxiety engaged in a specialized metabolic psychiatry program.”
In the coming years, metabolic therapies like nutrition, sleep, and exercise will be used to treat mental health conditions—approaches that are controversial or common sense, depending on your perspective.
The clinic of the future will integrate relational, experiential, energetic, and metabolic therapies to revolutionize the approach to mental and physical health.
Experiential therapies will recalibrate perceptions; energetic therapies will offer targeted brain stimulation, and metabolic approaches will address underlying physiological causes of mental health conditions.
This multifaceted approach promises to create a more effective and compassionate healthcare system, transforming how we understand and treat mental and physical well-being.
The future clinic is not just a place for treatment but a hub for comprehensive, personalized, and integrative care that prioritizes the well-being of the whole person.
This is obviously a bit of a strawman; these committee members clearly want what’s best for patients but operate from a Status Quo Bias. One way I’ve come to think about the perspective held by these committees is “Better the devil you know than the devil you don’t” and the uncertainty-tolerance with regards to new treatments is very low and even low wehn it comes to treatments with a well established cultural stigma and illegal status.
Tough to put Spravato in the same category as MDMA Assisted Therapy as the repeated rejection by the UK authorities is based on both the exorbitant cost (their opinion) of Spravato and the unconvincing clinical data of the currently available, FDA-approved drug.
Right now, these are distinct and discrete fields of research. While they may have different mechanisms, targets, and form factors, they are convening on a common theme: subjective well-being.
I choose this phrase—subjective well-being—intentionally because it covers the gamut of mood disorders, addictions, feelings of connectedness, safety, and self-esteem.
Part of the challenge that we have in midwifing this new paradigm is language. Depression is both a DSM diagnosis and common popular vernacular. Another challenge is the subjective—and thus unmeasurable—nature of the human experience.

No Comments